Patients addicted to opioids come to the emergency room with wounds so deep that their bones are exposed. Some have lost multiple limbs. And many ultimately leave the hospital with severe untreated skin lesions, against medical advice, claiming they cannot tolerate withdrawal from Trunk, the drug that caused the scars in the first place. are.
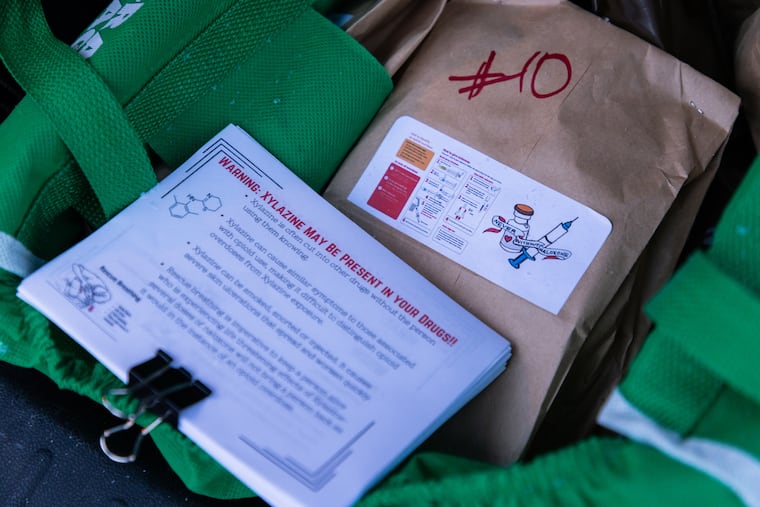
These stories come as doctors from Philadelphia’s major health system first compared notes on the medical effects of Trunk, the colloquial name for the animal tranquilizer xylazine, which has exploded in the city’s illicit opioid supply. That was one of the stories we shared.
At a weekend symposium hosted by Rothman Orthopedics and the Opioid Research and Education Foundation at Thomas Jefferson University, doctors discussed the cases of patients they have seen and limited information about how xylazine affects the body. The research was outlined.
“This has really changed the dynamics of the opioid crisis,” said Asif Ilyas, an orthopedic surgeon at Rothman who helped organize the event. “And Philadelphia is on the front lines.”
In recent years, doctors in Philadelphia have increasingly been treating wounds caused by xylazine. It was never approved for human use and is present in nearly all illegal opioids sold in the city. Health officials believe it was originally added to fentanyl to make the high last longer.
Xylazine also appears to cause severe skin lesions. At a symposium on Saturday, doctors said the drug is thought to be toxic to skin cells and constrict blood vessels, slowing the circulation of oxygen through the body and potentially slowing wound healing. .
Physicians who spoke emphasized the importance of collaboration to support patients who require care that goes beyond simply treating serious injuries.
“Scars are symptoms of a disease, not the disease itself,” says Jason Wink, a plastic surgeon at Penn Medicine.
Risks of prematurely discontinuing treatment
Physicians who treat comatose wounds also have to deal with the patient’s addictions. “This is a disease like any other disease,” Rachel Harross, director of toxicology and addiction medicine at Cooper University Hospital, told colleagues in other specialties.
Of particular concern is injured patients being discharged from hospital against medical advice before treatment is complete. In some cases, it may be because your doctor is not properly treating your withdrawal symptoms.
Avoiding wound treatment can have serious consequences. Catherine Woosley, head of orthopedic hand and neurosurgery at Cooper Hospital, suffered a wound covering most of her forearm and a number of other medical problems, including endocarditis, an infection of the heart valves. He spoke about a man who came to Cooper Hospital carrying a baby. Commonly seen in people who inject drugs.
The man was eventually discharged from hospital against medical advice, but returned a year later with his arm below the shoulder missing and some bone exposed. He told doctors the arm fell off on its own about six months ago.
Dr. Woosley did not say why the man was originally discharged from the hospital, but surgeons who treat uneventful wounds often work with addiction specialists and other social support services to provide better healing outcomes for patients. He emphasized the need for close cooperation.
“People are trying.”
At Temple University Hospital, doctors believe they have succeeded in developing a synthetic skin covering that can protect wounds for up to a year and allow them to heal even when patients are not ready to stop using drugs. Lisa Ray, Temple’s chief of burn surgery, said her goal is to reduce the risk of amputation for patients.
She spoke of a patient who sustained a wound that exposed the joint in his wrist, left the hospital multiple times, and continued to receive injections of medication. Doctors covered the wound with synthetic skin and the patient began to recover earlier this year. At a recent follow-up, the wound was almost healed, Ray said.
“Don’t give up on treating your wounds,” Ray said. “People are trying. This gives them time to find a way out.”
Other surgeons talked about how they treat patients with severe injuries that leave them unable to use their limbs.
Wink, a plastic surgeon in Pennsylvania, recalled a woman who suffered a severe injury to her forearm even though she hadn’t used drugs for three months. She told doctors she wanted to save the limb, but was relieved when it ultimately had to be amputated.
“Amputation can take the burden of the wound off the patient,” Wink said, urging careful consultation with patients, their families and other doctors before performing life-changing surgeries.
Creation of care guidelines
Physicians attending Saturday’s symposium said they are beginning to develop comprehensive recommendations for classifying and treating quiescent wounds. Earlier this year, health officials in Philadelphia also Guidelines released About wound treatment.
And addiction medicine experts say hospitals will also focus on follow-up care for patients on xylazine, ensuring they have enough medications, wound care supplies and connections to social services when they leave the hospital. He emphasized that it was necessary.
Ilyas said he was pleased that the first-of-its-kind symposium brought together so many doctors with different perspectives and specialties. “This is not a problem that can be addressed with surgery alone,” he says.
Early in the crisis, he said: “We have fundamentally failed to address the problem at hand, which is addiction, and this type of wound spans multiple surgical disciplines: orthopedics, burns, plastic surgery, general. Most of us haven’t trained for these injuries, so it’s important to exchange notes.”