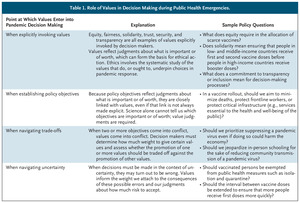
The Covid pandemic is posing enormous challenges to societies and healthcare systems around the world. Many of these challenges have been technical, such as developing effective vaccines and treatments. But one of the challenges that has proven to be the most thorny and controversial involves determining the ‘right’ course of action on many important issues. How to allocate scarce vaccines, whether to introduce mask and vaccine mandates, whether to limit travel, and how research participants are intended to test vaccines, to name a few directly infect. The “right” decision in these cases is neither a technical problem nor one that can be resolved by additional evidence. Rather, we need value judgments, and therefore ethics ( table 1).
Many policymakers and political leaders around the world have recognized that ethics play a central role in addressing these challenges, for example, the “fair and equitable” distribution of Covid vaccines. I am looking for But this realization rarely leads to ethically desirable outcomes. Some of the most important lessons from the pandemic, therefore, concern ethics and the effective integration of ethics into global health decision-making.
World leaders have frequently invoked ‘solidarity’, ‘fairness’ and ‘fairness’ during the pandemic, but clarifying these ethical codes, including how they should be implemented specifically. didn’t seem to be able to. For example, many calls for “fair and equitable” distribution of Covid vaccines across countries failed to characterize which distributions would be fair or equitable. Such calls indicated the need to provide more vaccines to low- and middle-income countries, but it is fair to say that how many vaccines should be provided to meet those objectives. or what sacrifices would be ethically justified on the part of high-income countries. help you navigate.
Covid is new, but the ethical issues it raises aren’t and needn’t be addressed first principleWe have extensive knowledge of relevant values and principles to guide policy during the global health emergency.1-3 Indeed, well-developed frameworks articulate ethical values for addressing health resource allocation, mandates, subject research, and other issues. These approaches have been informed by previous events considered public health emergencies of international concern, including the Zika epidemic, Ebola in West Africa, and H1N1 influenza. Ethical guidance can help make policy makers aware of this knowledge, navigate trade-offs between ethical values, and implement ethical principles in future health emergencies.
The Covid vaccine, for example, is not the first scarce medical resource that needs to be allocated. It was necessary to establish priorities within. These challenges have forced critical examination of practices, identification of unethical allocation schemes, and elucidation and critical evaluation of ethical frameworks and policies for the allocation of scarce medical resources.Four
 Fundamental values that influence the allocation of scarce medical resources.
Fundamental values that influence the allocation of scarce medical resources.
Analyzing existing knowledge on the one hand and the priorities established for allocating resources during Covid on the other reveals an agreement between the two on the importance of five substantive values when allocating resources will be , instrumental values, and equivalent moral concerns (see) Table 2). Explicit recognition of these values helps elucidate intrinsic ethical considerations, but further insight is needed to determine which values should prevail in a particular situation.
We argue that maximizing benefit and preventing harm should be given putative priority. However, this value should not have absolute priority. It must be balanced and shaped by the other four values. This helps clarify, for example, how much weight should be given to the distribution of benefits and harms among different populations. These values also impose constraints on profit maximization in accordance with an ethical commitment to social justice. For example, an already disadvantaged group should not be further disadvantaged by emergency resource allocation. Preventing harm to the most disadvantaged people is therefore of particular importance. Similarly, in public health emergencies, health care workers often get resource priority because of their instrumental value rather than because they are more valuable. Their work saves many other lives, thereby maximizing profits and preventing harm.
Other frequently invoked ethical principles, such as transparency, engagement, and response to evidence, are procedural. Unlike material values, they do not determine the allocation of resources, but can make such allocations more equitable. Don’t just clarify. The allocation scheme should also be translated into a mere policy that is faithfully implemented. For quotas, these policies take the form of prioritized strata of the population. Procedural principles shape and constrain the process of translating values into priority layers and implementing them into the world.
While it would be naive to expect unanimous consensus on scarce health resource allocations, mandates, or research challenges, there is no need to return to those debates when the fundamental values are already clear. Advancing this multivalent framework and existing ethical knowledge may not ‘solve’ these problems, but it will facilitate faster policy development and encourage policy makers to publicize the ethical basis of their policies. You will be able to tell Such communication should help improve awareness, trust and compliance.
But ethical values cannot apply themselves or resolve conflicts between them. Positioning ethics to inform decision-making in a meaningful way requires changes in the policy-making process. Ethics must be considered when initiating a response to a health emergency. Government policy should be expected to be explicitly ethical, not just evidence-based. In emergencies, policymakers look to epidemiologists and others to bring their expertise and experience to inform policymaking. They should also call on ethicists to inform coherent ethical responses.
How can this approach be operationalized?
Second, this function cannot be performed by a single token ethicist.As Covid has proven, many ethical issues involve the complex global and regional implications of pandemic planning and , and a competent team with complementary competencies and skills that can fully consider local impacts.
Third, before an emergency occurs, staff ethicists can use existing knowledge to anticipate common issues such as scarce resource allocations, missions, isolation protocols, and task studies. A vetted framework that incorporates well-accepted ethical values can then be elucidated. You can use these frameworks to create potential policies for your implementation. Ethicists can also translate these frameworks into checklists to ensure that relevant ethical considerations are addressed by policy makers when responding to emergencies.Five Staff ethicists solicit input on suggestions from experienced ethicists and members of the public (including those who have been disenfranchised) to refine a practical ethical framework and initial set of policy considerations. can.
Finally, ethics must be integrated into urgent decision-making. Ethicists need to be at the table when policy is formulated, rather than simply serving as an outside critic.
The world has not yet had time to fully unravel the lessons of Covid and apply them to future emergency preparedness. But policy makers must heed the lessons of the pandemic by understanding not only the technical but also the ethical aspects of all the challenges they face in emergencies. Start with your existing knowledge of the right values and principles to guide policy. and by ensuring that ethical expertise exists before emergency response is conceived and effectively integrated into decision-making. Achieving these goals will require sustained and focused efforts to strengthen ethical capacity in major global, national, and local public health organizations, academic institutions, and government agencies.