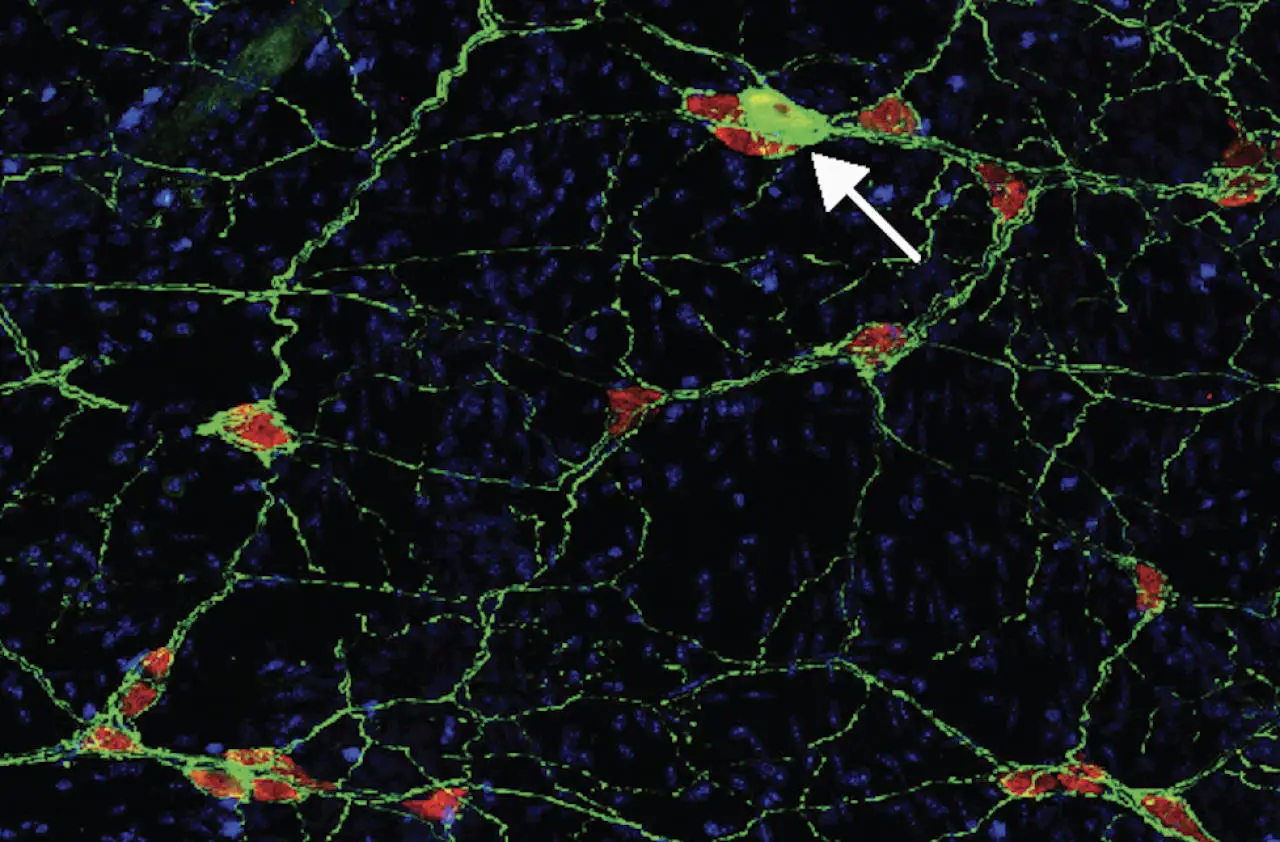
An autoimmune response in mice to proteins associated with Parkinson’s disease damages neurons in the gut, adding to the evidence that the disease may begin in the gut.Credit: David Sulzer, Columbia University Irving Medical Center
Ask any neurologist and they will tell you that Parkinson’s is a disease of the brain. The unmistakable signs of the disease, such as involuntary tremors, slow movement, and a feeling that the feet are stuck to the floor, are caused by the loss of neurons in areas of the brain responsible for regulating movement.
But a growing number of scientists theorize that the roots of this neurodegenerative condition may be traced back to the gut, where symptoms may appear long before neurological symptoms appear.
A new finding by Columbia University researchers David Sulzer, Ph.D., Dr. Doritan Agariou, and two of their graduate students provides further evidence to support this hypothesis, triggering early gastrointestinal changes in Parkinson’s disease. An immune attack indicating that things may have been misdirected.
“If this is the beginning of Parkinson’s disease in many people, we may be able to identify who has Parkinson’s disease before it reaches the brain, and hopefully stop it from progressing. says Sulzer.The new discovery was recently published in a journal neuron.
autoimmunity and gut
Originally proposed 20 years ago, the gut-first theory of Parkinson’s disease began to intrigue Sulzer after his own research pointed to the role of autoimmune responses in Parkinson’s disease.
In Parkinson’s disease, a protein called alpha-synuclein is misfolded and accumulates inside neurons, slowly poisoning the cells. Sulzer’s lab, working with immunologists at the La Jolla Institute of Immunology, found that some of the misfolded alpha-synuclein could also appear outside neurons, allowing neurons to enter the immune system. showed vulnerability to attacks from Immune attack may cause more severe damage to neurons than internal deposition of α-synuclein.
“The blood of people with Parkinson’s disease often contains immune cells that are ready to attack neurons,” says Sulzer. “But it’s not clear when or where they will be ready.”
It was an interesting possibility because the gut contains the same neurons and most Parkinson’s patients experience constipation years before brain symptoms appear and the disease is diagnosed. . To pursue this hypothesis, Sulzer collaborated with neuroimmunologist Agariou, who has expertise in mouse models for another neurological disease with autoimmune features: multiple sclerosis.
Immune response to α-synuclein causes intestinal symptoms
To see if and where an immune response to alpha-synuclein can cause disease, graduate students Francesca Galetti and Connor Monahan, supervised by Agarrieu and Sulzer, studied cell surface We generated the first mouse that can display fragments of misfolded α-synuclein. (Native mice do not have this ability). Then they injected the mice with alpha-synuclein and watched what happened in the brain and gut.
The researchers found no signs of Parkinson’s disease in the brain, but an immune attack on neurons in the gut that occurs in most Parkinson’s patients years before the disease is diagnosed. found to cause constipation and other gastrointestinal effects similar to
“This shows that an autoimmune reaction can cause what we believe to be the early stages of Parkinson’s disease, and strongly supports that part of Parkinson’s disease is an autoimmune disease,” Sulzer said. says.
The findings also raise the possibility that early detection and subsequent blocking of immune responses in the gut could prevent subsequent attacks on neurons in the brain and halt the progression of Parkinson’s disease.
Wanted: Mice with Parkinson’s Disease
However, at this time it is not clear just how big a role the immune system plays in the brain in Parkinson’s disease. The answer may become clearer if researchers can figure out why the brains of mice showed no signs of Parkinson’s disease.
The researchers hypothesize that immune cells in the mouse model fail to reach the brain because the animals are young and the blood-brain barrier has not yet weakened sufficiently with age for immune cells to pass through. . An open barrier or accelerated aging process can cause mice to develop gastrointestinal and cerebral symptoms.
“Our ultimate goal is to develop a Parkinson’s disease model in mice that mimics a human disease process that currently does not exist,” says Sulzer. “It will be very important in answering questions about this disease that cannot be explored in humans, and ultimately in developing better treatments.”
Reference: “Interaction of α-Synuclein Epitopes with HLA-DRB1∗15:01 Causes Intestinal Function in Mice Reminiscent of Precursor Parkinson’s Disease,” Francesca Galletti, Connor Monaghan, Nicholas Sloan, Jamie Bergen, Sanjid Shaharia, Song Woo Kim, Alessandro Sette, Tyler Cutforth, Ellen Kanter, Doritane Agariou, David Sulzer, August 18, 2023, neuron.
DOI: 10.1016/j.neuron.2023.07.015
This study was funded by the Coordination of Sciences Across Parkinson’s Disease through the Michael J. Fox Parkinson’s Research Foundation. National Institutes of Health; JPB Foundation. A donation to Neurology from the National MS Society, and Newport Equities LLC, the Walz family, and the PANDAS Network. Columbia University.