Opioid drugs such as morphine and fentanyl have a dual nature, like the Roman god Janus. A kind face brings pain relief to millions of patients, while a stern face triggers the crisis of opioid abuse and overdose. Nearly 70,000 people lost their lives In the United States alone in 2020.
Scientists like me who study pain and opioids They have sought ways to separate these two seemingly inseparable aspects of opioids. Researchers aim to design drugs that provide effective pain relief without the risk of side effects such as addiction or overdose.
One possible way to reach that goal is to understand the molecular pathways opioids use to exert their effects in the body.
How Do Opioids Work?
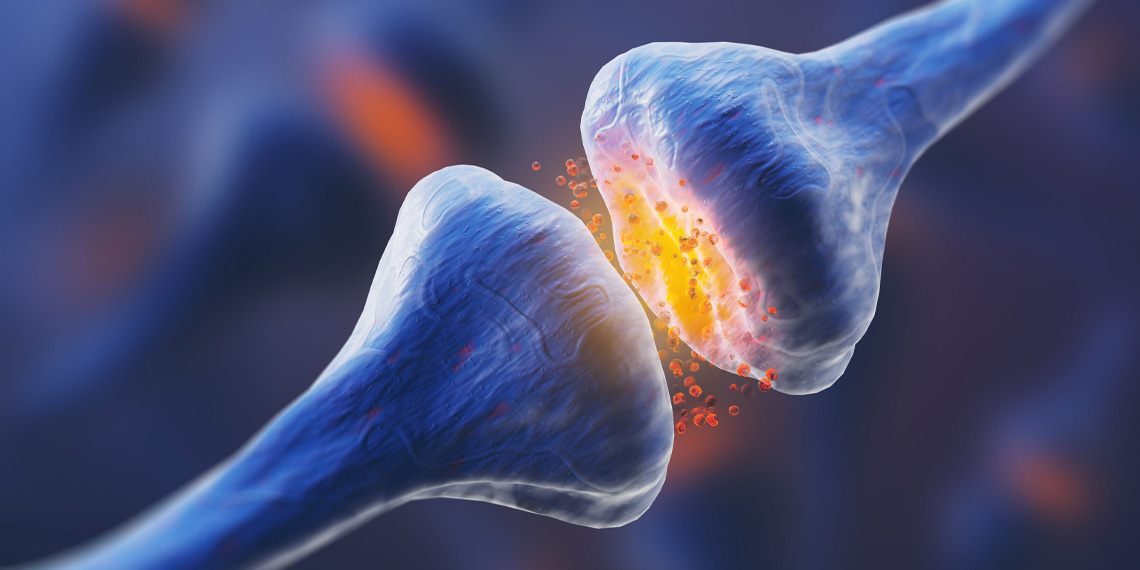
of the body’s opioid system is a set of neurotransmitters naturally produced by the brain that enable communication between neurons and activate protein receptors. These neurotransmitters include small protein-like molecules such as: enkephalins and endorphins. These molecules control a huge number of functions in the body, including pain, pleasure, memory, and digestive system movements.
Opioid neurotransmitters activate receptors such as: in many places It is present throughout the body, including pain centers in the spinal cord and brain, reward and pleasure centers in the brain, and entire neurons in the gut. Opioid neurotransmitters are typically released in small amounts at these precise locations, allowing the body to use this system in a balanced way to self-regulate.
Problems arise with opioid drugs such as morphine and fentanyl, especially when taken in high doses for a long period of time.these drugs move through the bloodstream Activates every opioid receptor in the body. Pain is relieved through pain centers in the spinal cord and brain. But when these drugs stimulate the brain’s reward and pleasure centers, they also produce a feeling of euphoria. lead to addiction with repeated use. Constipation and other common symptoms can occur when the drug reaches the intestines. side effects of opioids.
Targeting opioid signaling
How can scientists design opioid drugs that do not cause side effects?
One of the approaches my research team and I are taking is to understand how cells respond when they receive messages from opioid neurotransmitters.Neuroscientists describe this process as opioid receptor signaling. Just as neurotransmitters are the communication network in the brain, each neuron also has a communication network that connects receptors to proteins within the neuron. When these connections are established, they trigger certain effects, such as pain relief. Therefore, when a natural opioid neurotransmitter or a synthetic opioid drug activates an opioid receptor, it activates a protein in the cell that exerts the effect of the neurotransmitter or drug.
Opioid signaling is complex, and scientists are just beginning to figure out how it works. One thing is clear, though. Not all proteins involved in this process work the same. Some are more important for pain relief, others are more important for side effects such as: respiratory depressionor a decrease in respiratory rate that is fatal with an overdose.
So what if we target the “good” signals, such as pain relief, and avoid the “bad” signals that lead to addiction and death? Researchers are working on this idea in a variety of ways.In fact, in 2020 the U.S. Food and Drug Administration Approved the first opioid drug based on this ideaoliceridin is used as an analgesic with fewer respiratory side effects.
However, relying on just one drug also has its drawbacks. The drug may not work for everyone or for all types of pain. There may also be other side effects that appear only later. Many options are needed to treat all patients in need.
My research team is targeting a protein called heat shock protein 90, or Hsp90, with many functions within each cell. Hsp90 is Cancer field Over the years, researchers have developed Hsp90 inhibitors as treatments for many types of cancer.
We found that Hsp90 is also critically important in regulating opioid signaling. Block Hsp90 in the brain Blocking opioid analgesics. but, Block Hsp90 in spinal cord Increased opioid analgesia. Our recently published research reveals more details about exactly how this is done. Inhibiting Hsp90 reduces pain in the spinal cord.
Our study shows that manipulating opioid signaling through Hsp90 offers an avenue for improving opioid drugs. Combining her spinal cord-targeted Hsp90 inhibitors with opioid medications may improve opioid-induced analgesia while reducing opioid side effects. Improved analgesic effects reduce opioid intake and reduce the risk of addiction.we are Currently in development A new generation of Hsp90 inhibitors that may help achieve this goal.
There may be many avenues to developing improved opioid drugs without the nasty side effects of current drugs such as morphine and fentanyl. Separating the gentle and harsh faces of the opioid drug Janus could help provide the pain relief we need without addiction or overdosing.
This article is reprinted from conversation Under Creative Commons License.read Original work.