Researchers have discovered a bacterium that evades antibiotic treatment with an unprecedented trick.
Bacteria’s nasty talent for developing resistance to antibiotics is Rapidly Growing Health Threats. This ability is ancient origin and enable infection with drug-resistant bacteria MRSA When Gonorrhea Every year, 1.3 million people die worldwide.
These superbugs are also invading wildlife. dolphins etc. When bear.
crafty microbes steal genes from each otherrapidly communicating antibiotic resistance tactics: Strategies include directly inactivating antibiotics, preventing antibiotics from accumulating in the system, or altering antibiotic targets so that drugs become ineffective. included.
thanks for some Abuse of antibioticsSuperbugs have accumulated multiple resistance tactics, making them extremely difficult to treat.
“This new form of resistance is undetectable under conditions routinely used in pathology laboratories, making it very difficult for clinicians to prescribe antibiotics that effectively treat infections, and very difficult to treat.” It can lead to bad outcomes and even premature death.” I will explain Timothy Burnett, an infectious disease researcher at the Telethon Kids Institute.
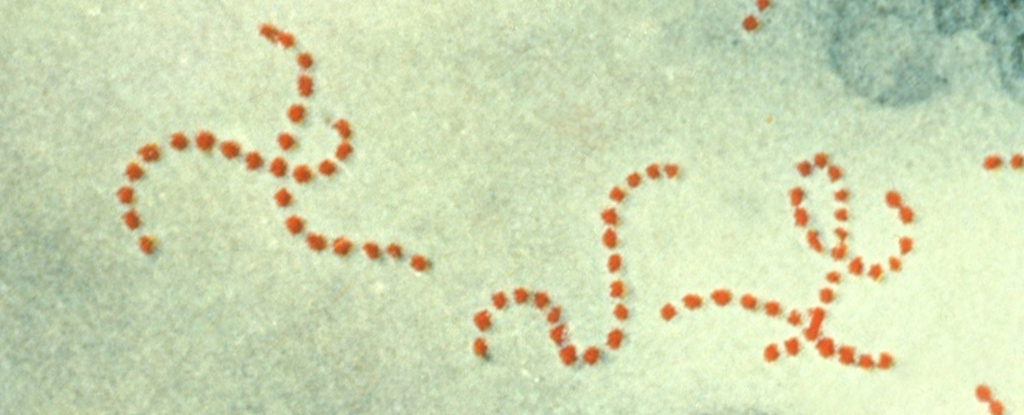
Kalindu Rodrigo, a microbiologist at the Telethon Kids Institute, and colleagues discovered this new mechanism while investigating its mechanism. Group A Streptococcus respond to antibiotics.
This bacterium commonly causes sore throats and skin infections, but can also cause systemic infections like scarlet. heat and toxic shock syndrome.
“Bacteria need to make their own folic acid to grow, which causes disease. Some antibiotics block the production of this folic acid to stop the bacteria from growing and treat the infection. ” I will explain Burnett.
“When we looked at antibiotics commonly prescribed to treat group A streptococcal skin infections, we discovered a mechanism of resistance. We have demonstrated for the first time the ability to take folic acid directly.”
yes Streptococcus You are getting already processed folic acid from outside your own cells. These molecules are abundant in our bodies.
This process completely bypasses the action of sulfamethoxazole, an antibiotic that inhibits folic acid synthesis in bacteria, thus rendering the drug ineffective.
Rodrigo and team identified at least one relevant gene, thfT. It encodes part of the folic acid harvesting system, as we too cannot produce folic acid and must obtain it from food.
Streptococcus Bacteria carrying this gene have therefore found a way to absorb folic acid and destroy sulfamethoxazole.
In the lab, Group A Streptococcus With no other available source of folic acid, we succumb to sulfamethoxazole antibiotics.
In this case, bacteria become resistant to antibiotics only when they are actually causing an infection in the body. This means that pathology laboratories do not yet have an easy way to detect this antibiotic resistance.
This mechanism suggests that antibiotic resistance is much more diverse than researchers previously realized, and underscores the need to establish. more diverse treatment against bacteria.
frameborder=”0″ allow=”accelerometer; autoplay; clipboard writing; encrypted media; gyroscope; picture-in-picture” allowfullscreen>“Unfortunately, this appears to be just the tip of the iceberg. We identified this mechanism in Group A Strep, but it could be a broader issue across other bacterial pathogens.” To tell Burnett.
Understanding these mechanisms is the first step to being able to test and counter them By prescribing other classes of antibiotics instead.
“Staying ahead of the antimicrobial resistance challenge is critical, and as researchers we need to investigate how resistance develops in pathogens and design rapid and accurate diagnostics and treatments. .” impulse Rodrigo.
This research Nature Communications.