Things to know:
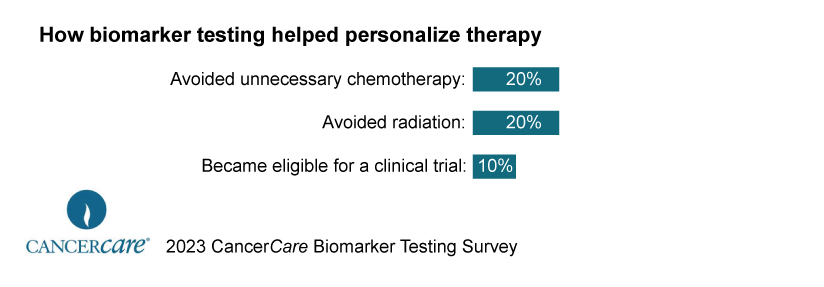
- Biomarker testing is a necessary tool for the advancement of precision cancer treatment. According to a new study published by cancer care, Biomarker Testing, a leading national cancer advocacy organization, helped physicians tailor treatment to nearly all (93%) of respondents who had been tested for cancer in the past three years. Two of her 10 cancer patients studied (20%) were able to avoid unnecessary chemotherapy and/or radiation, and 10% were included in clinical trials.
- Despite the significant and obvious benefits for the patients surveyed, 3 out of 10 (29%) of the respondents who underwent biomarker testing did not have insurance coverage for the test. Some survey respondents reported that they were initially denied biomarker test coverage and had to fight to get it covered. I had to find a way to ask for financial assistance to cover the cost of the tests.
Dealing with treatment delays in cancer treatment
Unfortunately, health insurance plans often limit cancer patients’ access to recommended biomarker tests, impose cumbersome preapproval protocols, or require affordable costs. may prevent or delay access to optimal treatment for cancer patients. A quarter (25%) of her cancer patients surveyed required prior approval, a significant obstacle to timely testing and treatment.
Biomarker testing has proven invaluable in identifying the most effective treatments for eligible cancer patients. This is to ensure that you get the right treatment at the right time while saving money and getting better results. However, there are still gaps in health insurance coverage for this important test. Patients and physicians have to go through many steps to obtain approval, and the sharing of costs can be prohibitive.
“Despite the fact that biomarker testing has dramatically changed the way cancer is diagnosed and treated, many insurers do not provide adequate coverage for the test,” said Patricia, CEO of CancerCare. says J. Goldsmith. “Employers who do not adequately cover this test in their insurance plans create a real risk that their employees will not receive the most effective and sometimes life-saving treatment.”
Eleven states have enacted or are about to enact legislation requiring biomarker testing for cancer patients to be included in their medical plans. Fortunately, an additional 18 states have introduced biomarker application laws, intended to require state-regulated public and private health plans to provide consistent coverage for this test. increase.
Biomarker testing is a matter of health care equity
Data from recent studies show that biomarker testing is becoming an increasing health care equity issue. A study published by the American Society of Clinical Oncology found significant disparities in biomarker testing rates between black and white lung and colorectal cancer patients, leading to disparities in participation in clinical trials and the most effective access to therapeutic treatment may be hindered. An important way to address these barriers, as recommended by medical experts, is to expand insurance coverage for biomarker testing.