From Philadelphia and the Pennsylvania suburbs to South Jersey and Delaware, what do you want WHYY News to cover? Please tell us!
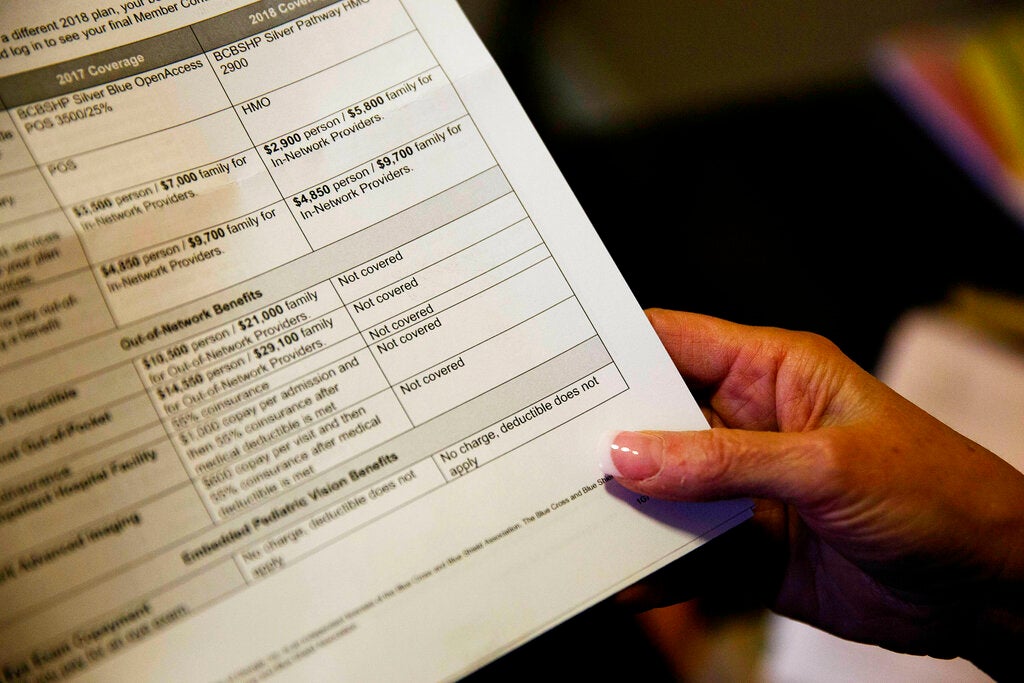
If you are denied coverage for a medical procedure or medication, you can usually appeal the decision directly to your health insurance company. But when that doesn't work, people are often left with limited options.
Now, a new program in Pennsylvania will take up these cases and give people new opportunities to challenge their insurance companies' decisions.
Pennsylvania Department of Insurance independent review program It was released this month. Assign eligible cases to a team of physicians, specialists, and other experts to determine whether an insurance denial was issued correctly or incorrectly.
If an independent review team contracted by the state determines that a patient was unfairly denied coverage, the health insurance company must reverse the denial and cover the service, medication, or treatment device.
“If people believe this is a service that should be covered, we'd say keep pushing,” said Shannen Logue, deputy commissioner of the state Department of Insurance. “We want people to know we're here. We've created a very easy solution online so people can quickly request it. [review]”
The program accepts cases submitted by residents with purchased health plans. through the penny, state Affordable Care Act markets. A person who purchases insurance directly from a company. Workers who obtain health insurance through their employer.
Eligibility will be determined within 5 days of someone submitting a request.
The program then assigns the case to a contracted independent review organization and team, followed by a 15-day “rest period” during which both the patient and the review team gather additional documentation and information related to the denial.
Logue said the review team has 45 days to analyze the incident. Most people receive their decision within 60 days.
The program has an expedited process for people who may be facing immediate life-threatening or serious health risks and need to make faster decisions.
The new screening program is the result of state law signed into law It was enacted in 2022 by former Governor Tom Wolf. It aimed to expand state-based screening services and support for people and their health insurance needs.