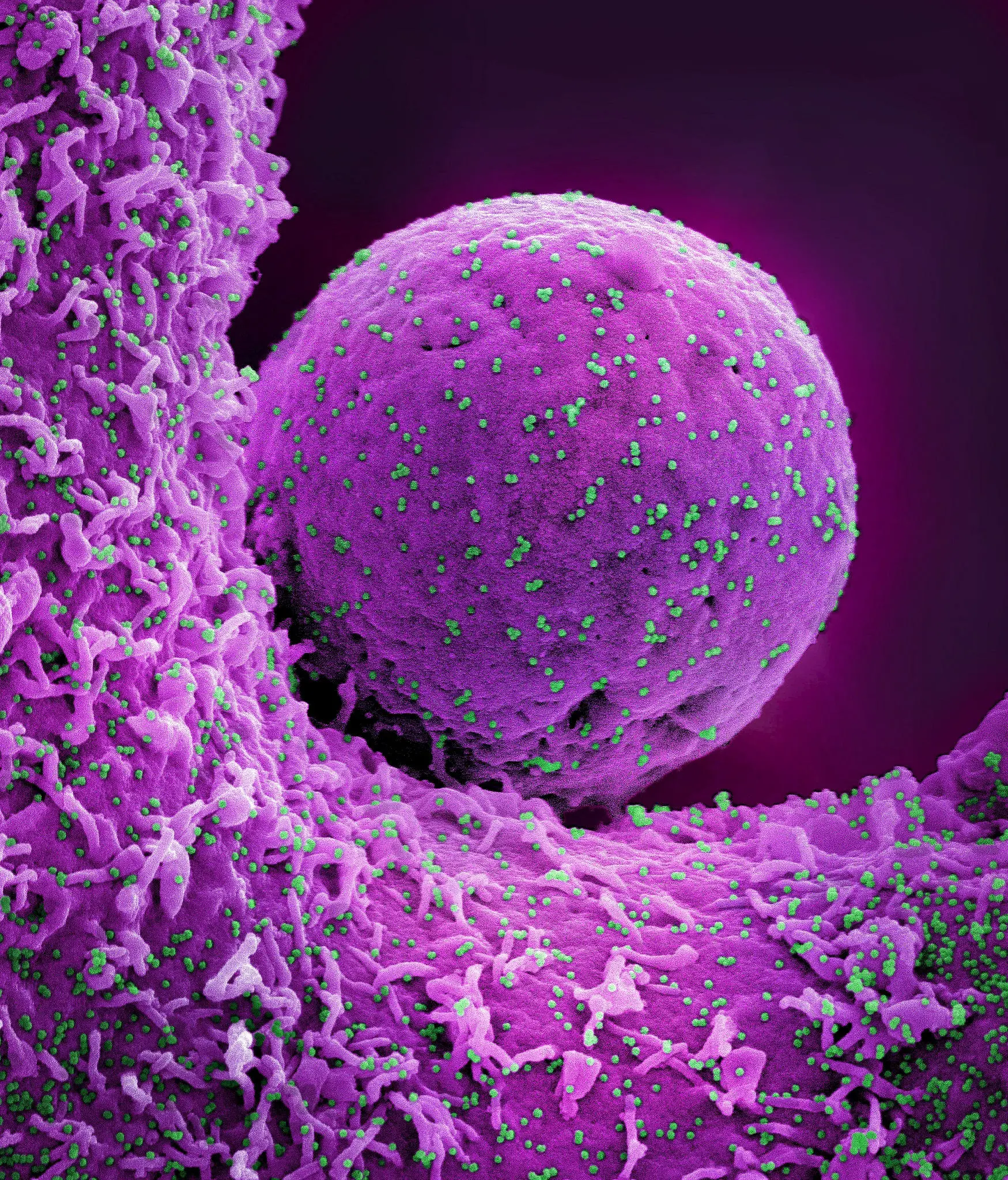
Colorized scanning electron micrograph of a cell (purple) infected with the Omicron strain of SARS-CoV-2 virions (green) isolated from an individual. Image taken at the NIAID Integrated Research Facility at Fort Detrick, Maryland. Credit: NIAID
Recent research reveals why younger children are less likely to become seriously ill COVID-19 (new coronavirus infection) Symptoms are more common than in adults.In this study, infected infants and young children SARS-CoV-2 demonstrated a strong and sustained antibody response to virus High levels of inflammatory proteins are present in the nose, but not in the blood. This immune response is in contrast to that typically seen in adults with SARS-CoV-2 infection. Through joint funding with the National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Healththe study is published in the journal cell.
Research methods and participants
The study included 81 full-term infants and infants whose mothers enrolled in a NIAID-supported cohort study at Cincinnati Children’s Hospital during their third trimester. The researchers trained mothers to take weekly nasal swabs from the time their infants were two weeks old. The team also took blood samples from the infants at regular intervals, starting at six weeks of age, when the children were infected with SARS-CoV-2, and in the weeks and months that followed.
These samples allowed scientists to study the immune responses of children before, during, and after their first exposure to the virus. Fifty-four of the children became infected and developed mild COVID-19 infection, while 27 who tested negative throughout the study served as matched controls. The children were between 1 month old and nearly 4 years old at the time of infection, and half were under 9 months old. The study included weekly nasal swabs taken from 19 mothers with COVID-19 and 19 healthy controls, as well as blood samples from 89 adults with COVID-19 and 13 healthy controls. was also included.
Main findings: Immune responses in children and adults
The researchers investigated various aspects of infant and adult immune responses to the virus through an approach called systems immunology. The study found that infants’ antibody responses to SARS-CoV-2 are different from adults’. Adults usually develop levels of antibodies against the virus that spike over a period of several weeks and then decline. In contrast, the infants and young children in the study had a sharp rise in the production of protective antibodies and remained high throughout the observation period of up to 300 days.
Scientists also found that the blood of adults infected with SARS-CoV-2 typically contains high levels of proteins called inflammatory cytokines, which are associated with severe COVID-19 infection and death, but that of infants and adults. They also discovered that it was not present in children’s blood. However, the children’s noses contained high levels of inflammatory cytokines and potent antiviral cytokines.
Meaning and recommendations
According to the researchers, these findings suggest that cytokines killed off SARS-CoV-2 infection at the site where the virus entered the children’s bodies, leading to milder COVID-19 infections in children. It may be possible to explain this. The findings also could lead to the creation of vaccine adjuvants that mimic the immune response observed in young children by stimulating sustained high antibody levels without causing dangerous excess inflammation in the blood. It suggests that.
Children aged 6 months to 4 years who received a COVID-19 vaccine before September 12, 2023 will receive the most recent COVID-19 vaccine, depending on their previous vaccinations and number of doses. Requires one or two vaccinations. Unvaccinated children aged 6 months to 4 years should receive their second or third dose of the latest COVID-19 vaccine, depending on which vaccine they receive.
Reference: “Multi-omic analysis of postnatal mucosal and systemic immunity to SARS-CoV-2” Florian Wimmers, Allison R. Burrell, Yupeng Feng, Hong Zheng, Prabhu S. Arunachalam, Mengyun Hu, Sara Spranger, Lindsay E. Niehoff, Devyani Joshi, Meera Trisal, Mayanka Awasthi, Lorenza Bellusci, Usama Ashraf, Sangeeta Khouri, Katherine C. Combins, Emily Yang, Michael Blanco, Kathryn Pellegrini, Gregory Tharp, Thomas Hagan, R. Sharon Cintraja, Tran T. Nguyen, Alba Grifoni, Alessandro Sette, Kari C. Nadeau, David B. Haslam, Steven E. Boersinger, Jens Lammert, and Holden T. Mecker. , Paul J. Utz, Taire T. Wang, Surender Khurana, Parvesh Khatri, Mary A. Sturt, Bali Prendran, September 29, 2023, cell.
DOI: 10.1016/j.cell.2023.08.044
Bali Pulendran, Ph.D., and Mary Allen Staat, MD, MPH, led the study. Dr. Purendran is the Violetta L. Horton Professor and Co-Director of the Institute of Immunology, Transplantation, and Infection at Stanford University in California. Dr. Sturt is the Kulkarni Endowed Chair in Infectious Diseases and professor of pediatric infectious diseases at Cincinnati Children’s Hospital.