Belo Lopez was excited to receive the new coronavirus vaccine. She is wary of the virus, and she still carries a mask and avoids indoor dining. So Lopez, 52, said she contacted her health care provider, Kaiser Permanente, as soon as she learned her vaccination had been approved last week. She didn’t have access to the vaccine yet, but a CVS pharmacy near her home in Los Angeles had an appointment for her. After calling her insurance company again to see if they would issue a refund, she booked her insurance.
A few days later, she received a message from CVS. Her plans were canceled.
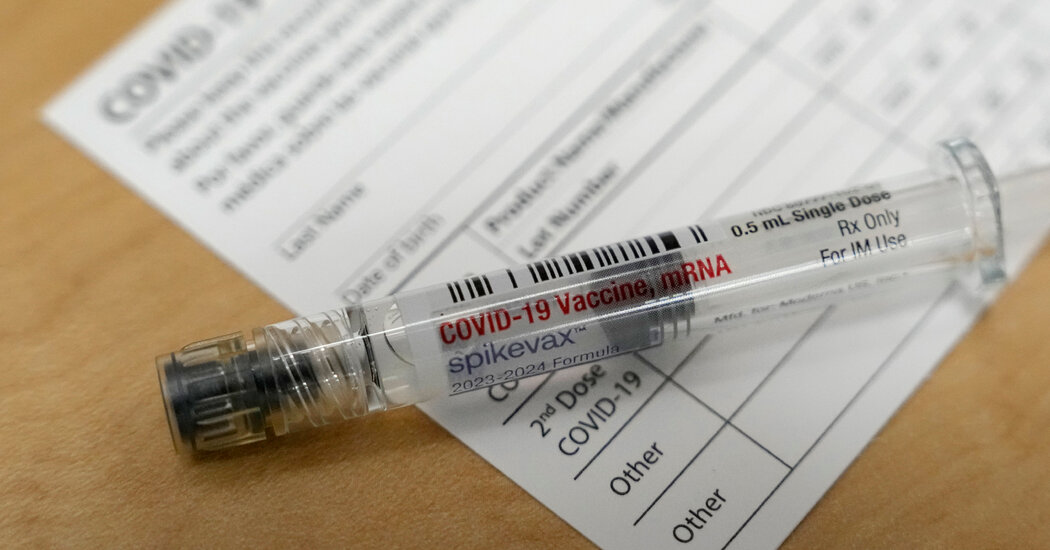
More than a week after a new coronavirus vaccine was approved and recommended for all Americans six months and older, some people are having trouble getting the shot. Insurance companies are refusing coverage, and some blame billing codes for the problem. Pharmacies are canceling some appointments because medicines are not delivered. And headaches over in-network and out-of-network coverage are adding to the confusion as the government no longer pays for everyone’s vaccines.
This is the first rollout of a commercial coronavirus vaccine since the pandemic began and marks the beginning of a new era of privatization of medicines. Millions of doses of vaccine have been shipped as hospitalizations rise. But like the early coronavirus vaccines, getting the shot into the arm has proven difficult.
U.S. Health and Human Services Secretary Xavier Becerra said at a press conference Wednesday that he had received his latest vaccine shot and said, “We have heard these stories and have contacted our insurance companies.” He said anyone with Medicaid, Medicare or private insurance should have the shot covered with no co-pay, and anyone without insurance can request a free shot at participating pharmacies. He emphasized. Bridge access program. “We are reaching out to pharmacists and working with them to make sure everyone understands how this works,” Becerra said.
Daniel de Sousa, head of the New York State Department of Health, said updated vaccine billing codes were not uploaded “in a timely manner,” delaying coverage for some people.
James Swan, president of AHIP, the National Association of Health Insurers, said insurers are working to resolve billing issues. Anthem Blue Cross Blue Shield announced Thursday that its payment system has been updated. A Cigna Healthcare representative said “the vast majority” of claims are being processed correctly.
Some of the country’s largest pharmacy chains acknowledged that the rollout has been difficult. CVS, Walgreens and Safeway pharmacies have had to cancel or reschedule some appointments due to delays in vaccine shipments, the companies said. Other providers delayed the availability of shots. Rite Aid said the new vaccine will be in stores by the end of this week. Kaiser Permanente said it will suspend most coronavirus vaccinations through next week.
Kit Longley, a Pfizer representative, said in an email that the company is not experiencing any vaccine shortages and has supplied millions of doses.moderna issued a statement The company said Thursday it is also shipping millions of updated vaccines and is working to help distributors ensure they are administered.
“The federal government will lead and drive vaccine supply and distribution through normal market channels as if it were another health care product,” said Lindsay Allen, a health economist at Northwestern Medicine. “I started getting pushed out,” he said.
Cynthia Cox, vice president of KFF, a health policy nonprofit formerly known as the Kaiser Family Foundation, said that despite billing code changes, some insurers are not updating their systems. expressed dissatisfaction with not being able to do so in time. It was released over a month ago. “This is an unprecedented situation,” she said. “I think there’s some understanding that there could be a problem. But at the same time, she said it’s been three years since this started and insurance companies and pharmacies have been preparing for months. is.”
KFF does not know how many people were affected, she said. “We only have anecdotes at this point, but we’re hearing so many stories that it feels like the problem is widespread.” It added that insurance is supposed to cover vaccines at out-of-network pharmacies. But Cox herself was unable to get the vaccine at her local Walgreens pharmacy in Silver Spring, Maryland, she said. She said the pharmacy was out of her network and she did not accept cash payments.
“There’s nothing I can do about it, even though this is exactly the field I work in,” she said.
What to do if coverage is denied
“Our message is simple,” said a representative from the Department of Health and Human Services. “If you are turned down for lack of coverage, please call your insurance company for more information about in-network coverage to receive the latest COVID-19 vaccine.” People were advised to book their vaccinations later if they had.
De Sousa, the New York State Department of Health representative, said people who paid out of pocket should contact their insurance company as soon as possible.