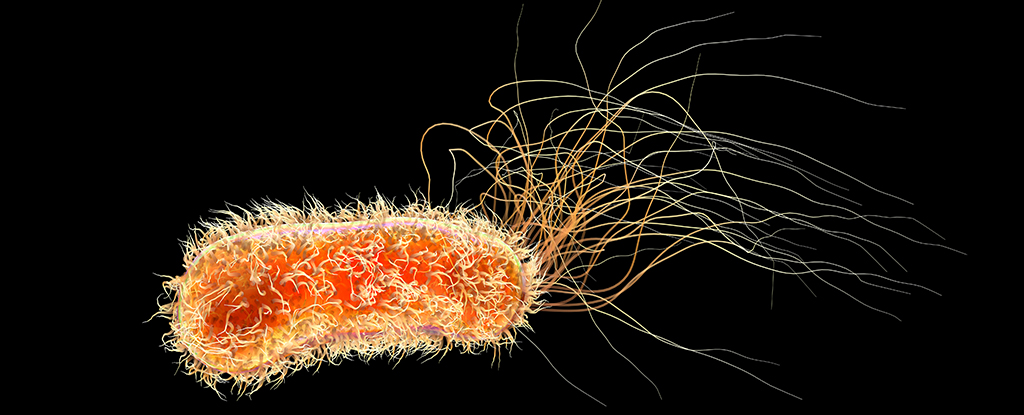
common Gram-negative Bacteria Pseudomonas aeruginosa They are truly cartoon villains among microbes.
This vicious killer has the ability to slip through our defenses and into our most sterile spaces. World Health Organization Priority 1 Pathogen List.
Most of us encounter these microbes in our everyday environments without any real harm, but under the right circumstances, they can quickly exploit tiny gaps in our defenses and cause explosive infections.
How such a ubiquitous microbe became such an opportunistic threat is a mystery, leading an international team of researchers to look a little more closely into the species’ evolutionary history.
A research group led by scientists from the University of Cambridge has constructed a genetic family tree of 596 closely related strains based on 9,829 bacterial samples taken from a range of human, animal and environmental sources around the world, some of which date back as far as 1900.
They found that just 21 strains of these bad bacteria are responsible for the vast majority of infections, and that the rapid evolution of these bad bacteria over the past two centuries has produced these dangerous infectious agents.
Over 500,000 people die each year as a direct result Pseudomonas aeruginosa This infection is particularly difficult to treat because the bacteria has an extensive antibiotic resistance toolkit.
Can survive As easy as jet fuel Similarly, in almost pure water, Pseudomonas aeruginosa There seems to be no limit to their adaptability. This extraordinary skill set is particularly problematic in healthcare settings, where even the most hygienic practices are not enough to prevent infection.
Hospitalized patients with chronic lung disease, e.g. Cystic fibrosis (CF) and Bronchiectasis are particularly susceptible to influence.
Indeed, the researchers found that some infectious strains of this bacterium have developed a strong affinity for CF patients, and upon closer inspection, they found that these strains have developed targeted methods to exploit the poor health of CF patients, allowing the microbe to evade destruction by the host’s immune system.
The CF-specific cells found a safe new space to survive among the immune cells tasked with eliminating them. Pseudomonas aeruginosa Strains continued to evolve by swapping resistance factors with each other, like recipes for a family lunch.
The discovery demonstrates the ability of pathogens to use their survival skills to establish new niches in extreme environments, giving them the space to quietly gather the tools they need to make new evolutionary leaps.
“From a clinical perspective, this study Pseudomonas” To tell Lead author Andres Flott is a respiratory biologist and director of the UK Cystic Fibrosis Innovation Hub at the University of Cambridge.
“The focus has always been on how easily this infection spreads between people with CF, but we’ve shown that it can also spread worryingly easily between other patients.”
Knowing how easily resistant pathogens can spread puts even more pressure on developing highly efficient screening and isolation measures.
Pseudomonas aeruginosa It’s unlikely to be an easy foe to defeat, but understanding this microbe’s strengths is essential to prevent it from evolving into an even more dangerous threat.
“Our research Pseudomonas “It teaches us new things about the biology of cystic fibrosis and reveals an important way to boost immunity against invading bacteria in this and other diseases.” To tell float.
This study Science.