 BBC
BBCDorothy Massa happily walks down a dirt road on a sunny afternoon with her baby clutched tightly on her back.
The 39-year-old from Malawi’s southern Choro district was in Kenya just six months ago to undergo life-saving radiation therapy.
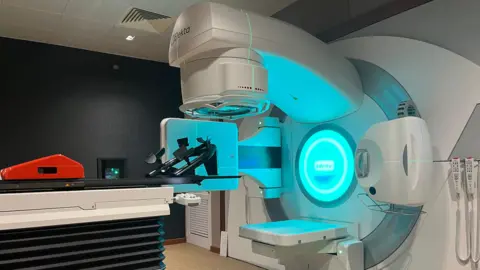
Other women with cancer may no longer need to travel abroad for treatment, as Malawi recently received the first such machine.
“When I was 13 weeks pregnant, doctors discovered cervical cancer and it was registered as an emergency case. They said the two were incompatible,” the mother of three told the BBC.
She said doctors in Malawi have advised her that patients can undergo surgery to remove the cancer, but the pregnancy will be terminated, or chemotherapy, but there is a risk that the baby will be born with disabilities. He said that there was.
She opted for chemotherapy until her baby was delivered by C-section without complications.
Her uterus was also removed during the same surgery.
Before her diagnosis, Masasa experienced lower abdominal cramps, bleeding, and a foul-smelling discharge that wouldn’t go away. At first, doctors thought it was a sexually transmitted disease.
But despite chemotherapy and surgery, she needed further treatment to cure her cancer, which was not available in Malawi until earlier this year.
She joined a group of 30 women taken to a hospital in Nairobi, Kenya, by aid agency Médecins Sans Frontières (MSF) to undergo radiation treatment to kill cancer cells.
It was her first time on a plane, so she was very anxious and reluctant to leave her newborn baby behind.
“But I encouraged myself that since I was going there for treatment, I should definitely go and get treatment, and that I would be able to go home healthy and happy.”
When the BBC visited the hospital, Masasa had lost weight and hair and was still weak from the effects of the treatment.
She is one of 77 patients flown from Malawi to Kenya for cervical cancer treatment since 2022.
Sixty years after gaining independence from Britain, Malawi just installed its first radiotherapy machine at the privately owned International Blantyre Cancer Center in March this year, marking a major step in the country’s healthcare system.
More machines will arrive in June and be installed at the still-under-construction National Cancer Center in the capital, Lilongwe.
Although Malawi still has a long way to go to provide comprehensive cancer care, it is further along than many other countries in the region.
in sub-Saharan Africa Over 20 countries They are unable to receive radiation therapy, which is essential to fighting cancer.
This means patients are forced to make expensive and arduous journeys for treatment.
Cervical cancer is 4th most common cancer among women worldwideAccording to the World Health Organization (WHO), it is estimated that in 2022 there will be 660,000 new infections and 350,000 deaths.
According to the World Health Organization, of the 20 countries with the highest rates of cervical cancer in 2018, all but one were in Africa.
This is due to a lack of access to preventive human papillomavirus (HPV) vaccines, appropriate screening and treatment, meaning many women delay seeking treatment.
Queen Elizabeth Central Hospital (QECH), Malawi’s oldest and largest government-owned treatment center, receives a huge number of cervical cancer patients from all over the country.
Dr. Samuel Meja, an obstetrician and gynecologist at the hospital, says cervical cancer is a big problem in most countries in the region.
“The situation is exacerbated by low access to testing and the scourge of HIV, which is raging across much of sub-Saharan Africa,” he says.
In 2018, Malawi was only second in southern Africa after Eswatini.had the highest incidence of cervical cancer in the world.
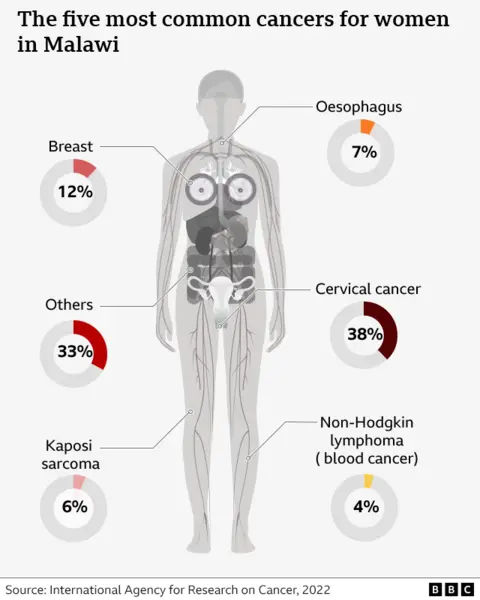
Outgoing WHO Regional Director for Africa Dr Matshidiso Moeti said a woman dies from cervical cancer every two minutes around the world. Africa accounts for 23% of deaths.
To reverse these grim statistics, large-scale campaigns are underway in Africa to vaccinate girls against HPV, which causes cervical cancer.
Reached Lesotho We vaccinated 139,000 girls with the HPV vaccine, achieving an unprecedented coverage rate of 93%.
However, there is a stigma against cervical cancer in various African countries, which affects the number of people who receive the vaccine.
In Zambia, for example, talking about gynecological matters is frowned upon.
Malawi has introduced cervical cancer screening, Dr. Meja said.
“This is a very simple strategy to identify women at risk and treat them before they become cancer patients. This is an investment we need to make as a nation before things get out of hand. ” he says.
Masasa is now back home in Malawi.
The treatment she received in Kenya gave her a new lease of life. Her hair grew back and she was able to walk around with her baby on her back, tend to the cows, and work in the fields.
She said she has no doubts about vaccinating her daughter because she now knows that cervical cancer is treatable and that the vaccine can help prevent cervical cancer in other women. Ta.
“I went through a difficult time with cervical cancer, and I don’t want my daughter to go through the same experience,” she says.
“There’s a big difference between me then and now. I’m so happy that I’ve healed.”

