overview: The gut microbiome appears to help regulate body temperature in both healthy people and those with life-threatening infections.
sauce: University of Michigan
What is considered normal body temperature varies from person to person, but overall, the average basal body temperature of the human body has been declining for unknown reasons since the 1860s. One study points to the gut microbiota as a potential regulator of body temperature, both in health conditions and in life-threatening infections.
Led by Robert Dixon, M.D., and his colleagues at UM Medical School, the study used health record data from patients hospitalized with sepsis and mouse experiments to study the mix of bacteria present in the gut, temperature fluctuations, and We examined interactions between health outcomes. .
Sepsis, the body’s response to life-threatening infections, can cause dramatic changes in body temperature, the trajectories of which are associated with mortality.
works published in American Journal of Respiratory and Critical Care Medicine In 2019, it was demonstrated that temperature responses in patients hospitalized with sepsis differed significantly and that this variation was predictive of patient survival.
“There’s a reason temperature is a vital sign,” says Cale Bongers, MD Ph.D., a clinical instructor in internal medicine and lead author of the study. “It’s easy to measure and gives us important information about the inflammatory and metabolic state of the body.”
However, the cause of this temperature change in both sepsis and health remains unclear.
“We know that the temperature response is important in sepsis because it is a strong predictor of who will live and who will die,” Dickson said. “But we don’t know what’s causing this variability, and if we can fix it to help our patients.”
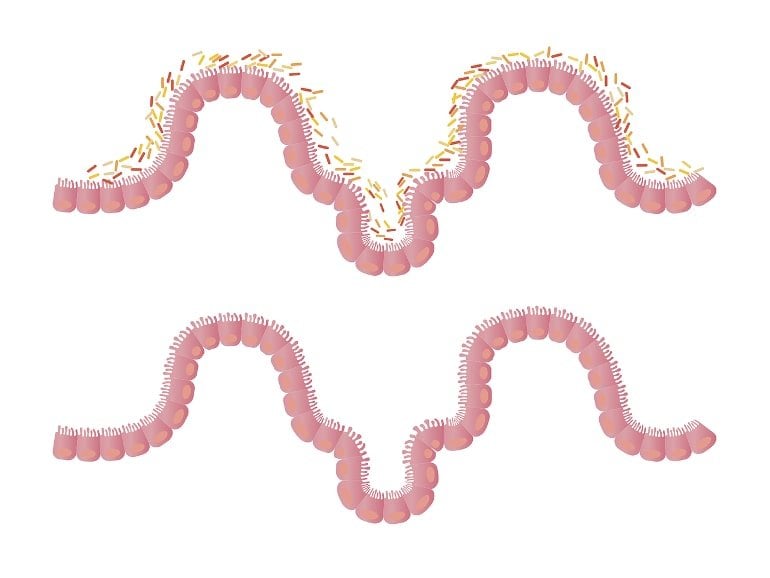
To understand the sources of this variability, the team analyzed rectal swabs from 116 hospitalized patients. The patient’s gut microbiome was significantly altered, which was identified as a potential cause of the alteration.
“Undoubtedly, our patients have more variation in their microbiome than in their genetics,” Bongers said. “Any two patients are more than 99% identical in their genome.” However, in gut bacteria there may be literally 0% overlap.”
The authors found that this variation in gut bacteria correlated with temperature trajectories in hospitalized patients. In particular, common bacteria of the Firmicutes phylum were most strongly associated with increased febrile responses. These bacteria are common, vary from patient to patient, and are known to enter the bloodstream and produce important metabolites that affect the body’s immune response and metabolism.
To confirm these findings under controlled conditions, the team used a mouse model to compare normal mice with genetically identical mice lacking the microbiome. Experimental sepsis caused drastic changes in temperature in conventional mice, but had blunt effects on temperature responses in germ-free mice. strongly correlated with the same bacteriaceae (Lachnospiraceae) found in
“We found that the same type of gut bacteria explained the temperature changes in both the subjects and the experimental mice,” Dixon said. “This gave us confidence in the validity of our findings and a goal to understand the biology behind this discovery.”
Even when healthy, mice without a microbiome had a lower basal body temperature than conventional mice.
This study highlights an underestimated role of the gut microbiota in body temperature and may explain the decline in basal body temperature over the past 150 years.
“Although it has not been definitively proven that changes in the microbiome explain the decline in human body temperature, we think it is a reasonable hypothesis,” Bongers said. “Over the past 150 years, human genetics have not changed meaningfully, but changes in diet, hygiene and antibiotics have had a profound impact on gut bacteria.”
Further research is needed to understand whether targeting the microbiome to regulate body temperature can help alter outcomes in patients with sepsis.
About this neuroscience research news
author: press office
sauce: University of Michigan
contact: Press Office – University of Michigan
image: image is public domain
Original research: closed access.
“Gut microbiota regulate body temperature in both sepsis and healthCale S. Bongers and others American Journal of Respiratory and Critical Care Medicine
overview
Gut microbiota regulate body temperature in both sepsis and health
basis: In patients with sepsis, changes in temperature trajectory predict clinical outcome. Normal body temperature in healthy people varies and has been consistently declining since the 1860s. The biological basis of this temperature change in disease and health is unknown.
Purpose: To establish and investigate the role of the gut microbiota in regulating body temperature.
Method: We performed a series of translational analyzes and experiments to determine whether and how variations in gut microbiota explain body temperature variations in sepsis and health conditions. The patient’s temperature trajectory was studied using electronic medical record data. We used 16S ribosomal RNA gene sequencing to characterize the gut microbiota of hospitalized patients. Intraperitoneal lipopolysaccharide in mice was used to model sepsis, and antibiotics, germ-free and gnotobiotic animals were used to modulate the microbiome.
Measurement results and main results: Consistent with previous studies, we identified four temperature trajectories in patients admitted with sepsis that predicted clinical outcome. In another cohort of 116 hospitalized patients, we found that the composition of the patient’s gut microbiota at admission predicted the trajectory of body temperature. Compared with conventional mice, germ-free mice had reduced temperature loss during experimental sepsis. Among conventional mice, the heterogeneity of temperature responses in sepsis was strongly explained by variations in the gut microbiota. Both healthy germ-free and antibiotic-treated mice had lower basal body temperatures compared to controls. consistently related.
Conclusion: The gut microbiota is a key and understudied target for modulating physiological heterogeneity in sepsis, as it is a key regulator of body temperature fluctuations in both health and critical illness.