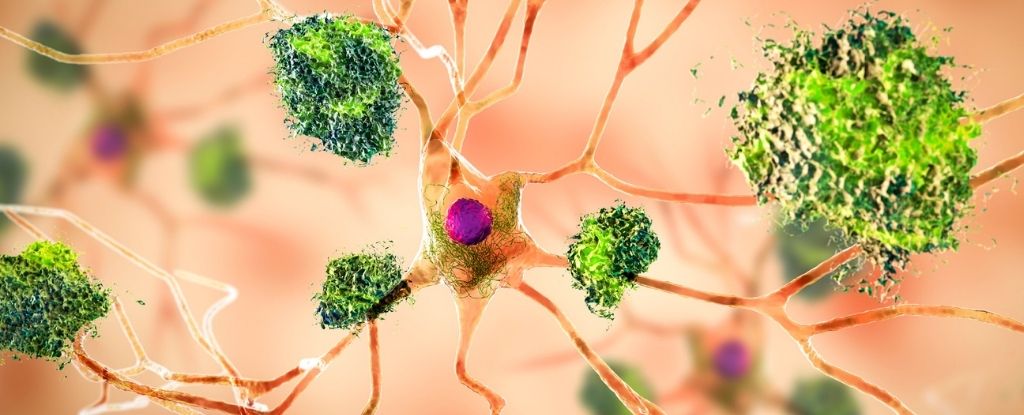
A common type of fungus has now been shown to invade the brains of mammals and cause toxic amyloid plaques, such as those associated with Alzheimer’s disease.
Although the findings were made in mice, the study suggests that key features of some neurodegenerative conditions may arise from sources other than the brain.
Amyloid protein clumps that appear between neurons are strongly associated with Alzheimer’s disease and are generally thought to be a result of endogenous stress or inflammation in the brain.
But in recent years, scientists have detected Common fungal symptoms known as candida albicans, Dissected brains of people with other neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease.
This allows foreign infections to enter the mammalian brain, triggering an innate immune response that can help destroy the pathogen, but if done poorly can lead to Alzheimer’s-like symptoms. Some people claim that.
To further explore this idea, an international research team led by experts at Baylor College of Medicine in the US turned to mice.
Previously in the same lab at Baylor University found The mouse was infected with C. albicans Memory loss was observed, which resolved after the fungus was removed.
Their new research is now investigating the molecular basis of that effect, primarily through “test tube” experiments.
First, researchers injected C. albicans It penetrates directly into the mouse brain. After 4 days, the mice were euthanized and their brains were used for further analysis.
Several brain slices were imaged and some cells were cultured on plates.
The findings suggest that:Because it’s in your brain, C. albicans It can trigger two neuroimmune mechanisms. One activates immune cells to suppress the fungus, and the other activates immune cells to completely eliminate the invader.
The first mechanism involves fungal enzymes called Saps that increase the leakiness of the blood-brain barrier. This allows fungal cells to enter, which can flow into the brain through the body’s bloodstream.
At the same time, the sap also breaks down amyloid beta-like proteins, similar to those that form plaques in Alzheimer’s brains, and activates cleanup cells called microglia.
The second mechanism involves the secretion of another fungus, which also triggers microglia, which in turn targets the fungus for clearance.
Combining both immune pathways,Very effective in resolving acute symptoms C. albicans“Infection in the brain of a healthy mouse, usually it occurs Approximately 10 days.
But not all brains are young and healthy. When researchers deliberately disrupted microglial responses in the brains of mice, they found: C. albicans The infection lasted significantly longer.
“If you remove this pathway, the fungus is no longer effectively cleared in the brain.” To tell Yifan Wu of Baylor College of Medicine;
Clumps such as amyloid beta found in mouse brains appear to be sentinels against invading pathogens, but their presence may be harmful in the long term if these clumps are not properly cleared by microglia. It may become clear.
For now, this is just a hypothesis, but it is consistent with recent research showing that amyloid-beta plaques are a sequela of Alzheimer’s disease and not the original trigger for cognitive decline.
This may be why treatments targeting these plaques in humans have little success.
“This study may contribute an important new piece of the puzzle regarding the development of Alzheimer’s disease.” To tell said David Colley, an immunologist who led the study at Baylor University.
“The leading idea is that these peptides are produced endogenously, with our own brain proteases breaking down amyloid precursor proteins and producing toxic amyloid beta peptides.”
But that may not be the case after all.
Although more research needs to be done in both live animal models and human cells, Baylor University researchers believe their initial experiments could lead to innovative treatments for cognitive decline in the future. I hope there will be.
This study cell report.