Obesity experts say about 20% of patients (1 in 5) may not benefit reliably from new drugs.
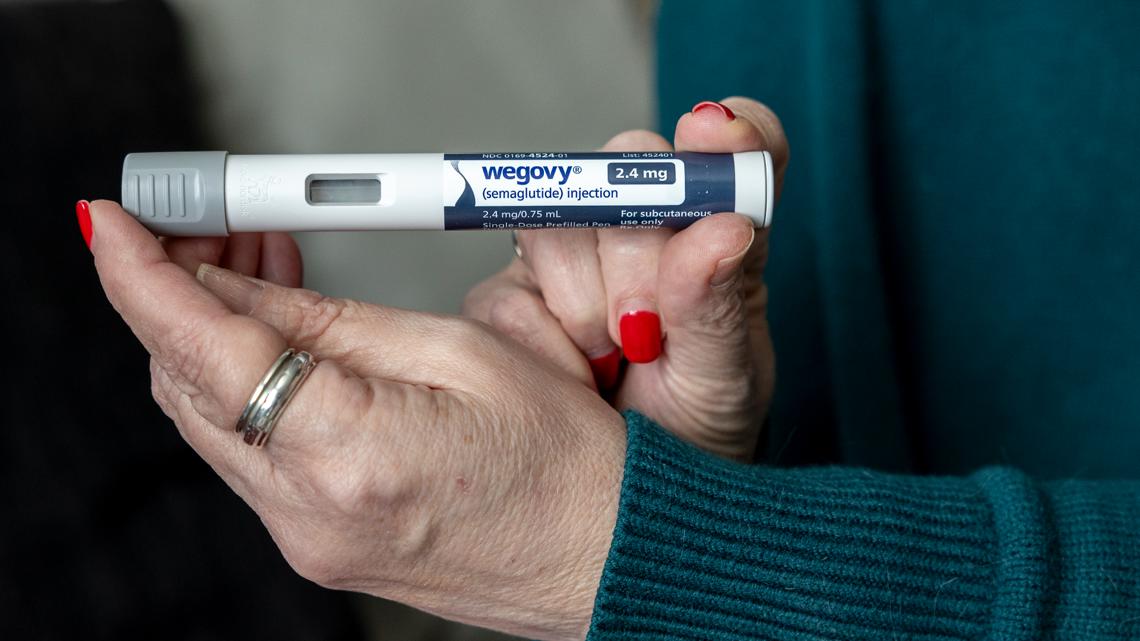
WASHINGTON, DC — Unlike many people; scramble Daniel Griffin has had no trouble getting his hands on the blockbuster weight-loss drugs Ozempic and Wegoby in recent years.
The 38-year-old information technology worker from New Mexico had a prescription. Her pharmacy had medicine in stock. and she health insurance We covered all but $25 to $50 of monthly costs.
For Griffin, the most difficult part of using the new drug wasn’t access. it is, highly advertised drugs It didn’t do much for her.
“I’ve been using Wegovy for a year and a half and I’ve only lost 13 pounds,” said Griffin, who watches her diet, drinks plenty of water and exercises regularly. “I did everything right, but I wasn’t successful. It’s depressing.”
In clinical trials, most participants who took Wegovy or Mounjaro to treat obesity lost an average of 15% to 22% of their body weight, often up to 50 pounds or more. However, approximately 10 to 15 percent of patients in those trials were “nonresponders” who lost less than 5 percent of their weight.
With millions of people currently using the drug, several obesity experts told The Associated Press that perhaps 20% of patients (1 in 5) may not respond well to the drug. he said. Doctors say this is a little-known consequence of the obesity drug boom and are warning eager patients not to expect one-size-fits-all results.
“It’s important to explain that different people react differently,” said Dr. Fatima Cody Stanford, an obesity expert at Massachusetts General Hospital.
This drug is known as a GLP-1 receptor agonist because it mimics a hormone in the body known as glucagon-like peptide 1. Genetics, hormones, and variations in how the brain regulates energy can all influence weight and a person’s response to medications. Stanford said. Medical conditions such as sleep apnea can interfere with weight loss, as can common medications such as antidepressants, steroids, and birth control pills.
“This is a brain disease,” Stanford says. “The functional impairment may not be the same from patient to patient.”
Despite these precautions, patients often become upset when they begin receiving weekly injections, but the number on the scale remains largely unchanged.
“It can be devastating,” says Dr. Katherine Saunders, an obesity expert at Weill Cornell Medicine and co-founder of the obesity treatment company FlightHealth. “When expectations are this high, there is so much room for disappointment.”
Griffin had battled obesity since childhood and wanted to use Wegovy to lose 70 pounds. The drug helped reduce her appetite and lower her risk of diabetes, but her weight showed little change.
“It’s a roller coaster of emotions,” she said. “We want it to work just like everyone else.”
The medicine is usually prescribed It also involves changes in eating habits and lifestyle.
Dr. Jodi Duchey, an endocrinologist at Beth Israel Deaconess Medical Center, says it’s usually obvious within a few weeks whether someone will respond to a drug. Weight loss usually begins immediately and continues as the dose is increased.
For some patients, that doesn’t happen. Some people may have to stop taking the drug due to side effects such as nausea, vomiting and diarrhea, Duchey said. In this situation, patients who were counting on new drugs to lose weight may think they have no choice.
“I tell them, this is not game over,” Dusha said.
It may be helpful to try a different version of a new class of drugs. After not responding well to Wegovy, Griffin began using Zepbound, which targets additional hormonal pathways in the body. After 3 months of using this drug, she lost 7 pounds.
“I hope it’s slow and steady,” she said.
Experts say some people respond better to older drugs. Changing your diet, exercise, sleep, and stress habits can also have a big impact. Understanding what works typically requires a doctor trained in obesity treatment, Sanders said.
“Obesity is a very complex disease and needs to be treated very comprehensively,” she said. “Even if the medications we prescribe don’t work, we always have a backup plan.”
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Education Media Group. AP is solely responsible for all content.