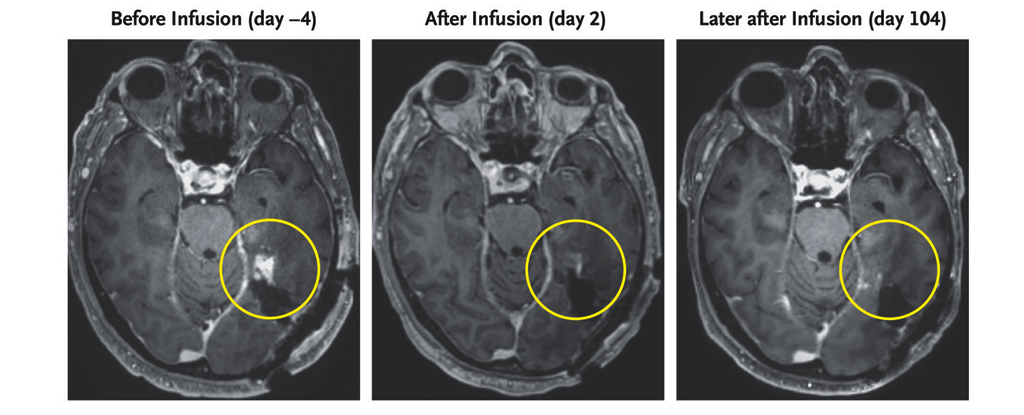
A brain scan of a 72-year-old man diagnosed with a very aggressive form of cancer known as . glioblastoma They revealed a significant regression in tumor size within days of receiving an injection of the innovative new treatment.
Although the results of two other participants with similar diagnoses were somewhat less positive, the success of this case still bodes well for the search for ways to effectively treat this currently incurable disease. be.
Glioblastoma is usually as deadly as cancer. Once emerging from supporting cells within the central nervous system, it can rapidly develop into a malignant tumor, causing symptoms such as: Up to 95% of patient’s life Within 5 years.
Researchers at the Massachusetts Comprehensive Cancer Center in the US doubted that treatments based on a patient’s own immune system. CAR-T cell therapycan be successful even when other treatments have failed.
The superior ability of CAR T-cell therapy, approved to treat blood cancers, to sniff out cancer cells could offer an advantage in destroying glioblastoma.
The patient’s T cells are collected and re-engineered to recognize identifying surface markers on the outside of cancer cells before being returned through an IV drip. In other words, CAR T-cell therapy is akin to hiring a local bounty hunter to silently scour the alleys. Of a wanted villain.
One marker that is widespread in a range of glioblastomas, mutant It is a type of protein called epidermal growth factor receptor (EGFR), which is a potential target for CAR T cell therapy. Unfortunately, glioblastomas come in many disguises, making the reengineering process extremely difficult.
To overcome this, researchers have discovered a way to encourage CAR T cells to produce antibodies that seek out the non-mutated form of EGFR. These proteins are not normally expressed in brain cells, but are found in cancer cells, providing additional identification features to recruited bounty hunters.
Preclinical clinical trials have shown that T cell-associated antibody molecule (TEAM) therapy works as expected at the tumor site, recruiting other regulatory T cells to join the fight.
Intraventricular CARv3-TEAM-E T Cells in Glioblastoma Patients (INCIPIENT) is a phase 1 clinical trial aimed at evaluating the safety of the process and its potential as a treatment.
Only three patients were recruited, all of whom were diagnosed with a type of glioblastoma that expresses mutant EGFR.
The first patient was a 74-year-old man who received standard medications and radiation therapy for his tumor, but the tumor returned a year later. The day after receiving the infusion of CARv3-TEAM-E T cells, an MRI scan showed a significant reduction in the size of the mass, and the prognosis seemed favorable.
Just a few months later, the patient was back on the operating table, and subsequent scans revealed that the cancer had grown again.
The same was true for a 57-year-old woman with a large glioblastoma in the left hemisphere. Her tumor had almost completely regressed five days after treatment, but just one month later she showed signs of cancer recovery.
In the third participant, who was 72 years old, the cancer had shrunk with no signs of recurrence, and side effects were limited to fever and temporary nodules in the lungs, leading researchers to consider a new immunotherapy approach. I am optimistic that there is a basis for continuing the search.
“Our work with CARv3-TEAM-E T cells provides proof of principle that CAR T cells can be used to simultaneously target multiple surface antigens and confirms that EGFR is a suitable immunotherapeutic target in glioblastoma. “We confirmed that this is the case,” the research team said. I wrote this in the published report:.
Without knowing the long-term prognosis for any patient, it is premature to describe the treatment as curative. But with further research and additional clinical trials, CAR T-cell therapy could offer a glimmer of hope to at least some patients diagnosed with the most deadly cancers.
This research New England Medical Journal.