A new study points to decreased levels of a well-known chemical messenger in people with long-term COVID-19 infections, and identifies a pathway linking several possible causes of the disabling condition. Ta.
the same as There are other researchers in front of them.University of Pennsylvania immunologist Andrea Wong and colleagues have discovered a clear biology that may explain the puzzling combination of up to 200 potential symptoms that long-term COVID-19 patients can experience. We explored changes in
Research has come a long way since the early days of the pandemic. deciphering possible causes Prolonged COVID-19 infection can persist for months or even years after acute SARS-CoV-2 infection has subsided.
But this growing body of research also paints a somewhat troubling picture of overlapping underlying causes. That is, increased blood clotting, residual viruspersistent inflammation, and nervous system dysfunction are just some of the working theories that seek to explain the development of long-term COVID-19 infections.
The results of this new study suggest that four of these mechanisms may be interconnected and may explain cognitive impairment and memory loss in patients with long-term COVID-19 infection. report. Not only that, but the study’s findings, if replicated in a larger cohort, could point the way to possible treatments.
Researchers analyzed blood samples from 58 patients with long-term coronavirus infections and found several differences that separated them from the 30 who had fully recovered.
People who have been suffering from the new coronavirus infection for a long time, serotonin, a chemical messenger best known for its mood-enhancing role, among other functions related to memory, cognition, and sleep. Long-haulers also shed virus particle debris in their flights.
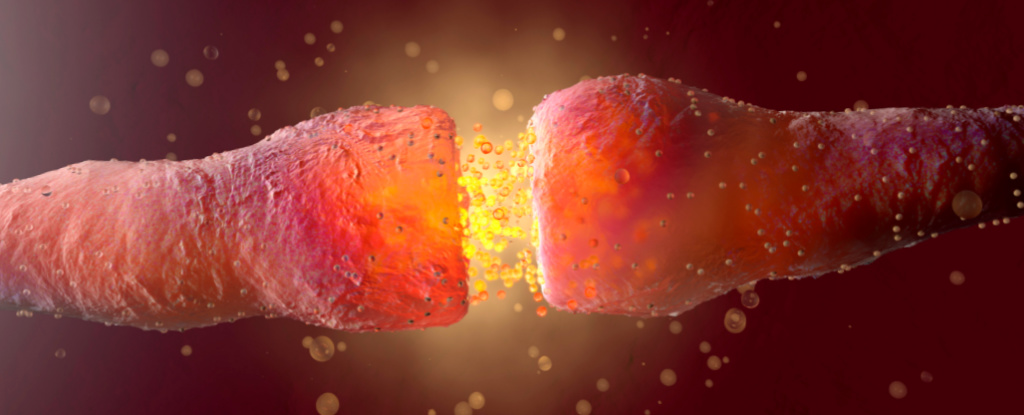
Using a combination of animal models and organoid cultures, the research team has assembled a pathway that may link serotonin deficiency in the gut, where most serotonin is normally produced, to effects in the brain.
The link they propose is: lingering viral material may trigger the body’s immune system to shed it. interferona group of signaling proteins involved in antiviral defense.
This causes inflammation and limits the absorption of tryptophan, an amino acid used in the production of serotonin in the intestines.
Persistent inflammation also damages platelets, blood cells that are involved in blood clotting and carry serotonin throughout the body.
When there is less circulating serotonin, cell activity decreases. vagus nervethe body’s superhighway that sends signals between the brain, gut, and other organs.
“Our findings demonstrate that some of the current hypotheses regarding the pathophysiology of long-term COVID-19 infection (viral reservoir, persistent inflammation, hypercoagulability, vagal dysfunction) are linked by a decrease in serotonin. “This suggests that they may be connected by a single pathway,” said Maayan Levy of the University of Pennsylvania. Microbiologist and lead author of the study, explained on social media.
In mice, the reduction in serotonin levels and decreased vagus nerve activity caused by the virus infection caused the animals to perform worse on memory tests.
But surprisingly, memory impairments that resemble, but do not clearly replicate, the cognitive impairments of long-haulers may be prevented once serotonin levels are restored.
More human studies are needed to test these suggestions. Future research will need to understand why some people in the second cohort of long-term COVID-19 patients, who probably had milder symptoms, did not have lower serotonin levels.
“We hope that our findings will influence clinical research that uses these insights to develop new tools for the long-term diagnosis, monitoring and treatment of COVID-19,” Levy said. Ta. Added. “They are needed very urgently.”
This research cell.