February 6, 2023
4 minute read
Source/Disclosure
Disclosure:
Pittas reports that the American Diabetes Association and the NIH supported the study. Dr. Pittas also reports that he is co-chair of the Endocrine Society’s Clinical Practice Guidelines for Evaluation, Treatment and Prevention of Vitamin D Deficiency. See research for relevant financial disclosures of all other authors.
Vitamin D was effective in reducing diabetes risk in prediabetic adults, according to the results of a systematic review and meta-analysis published in . Chronicle of internal medicine.
“Observational studies strongly and consistently support an inverse relationship between blood 25-hydroxyvitamin D levels and risk of type 2 diabetes. The question of whether or not to do so remains open.” Anastasios G. Pittas, MD, MS, Written by Professor of Medicine, Chief of Endocrinology, Director of the Endocrinology Fellowship Program, and colleagues at Tufts Medical Center.
Data source: Pittas AG, et al. uninterneddoi:10.7326/M22-3018.
Investigators conducted a systematic review and meta-analysis of trials testing the effects of oral vitamin D and placebo on new-onset diabetes in prediabetic adults. Ultimately, the analysis included her 4,190 participants from his three randomized clinical trials. 44% of the participants were female, 51% were Caucasian, and the average age was her 61 years.
The researchers primarily sought to understand the time to onset of new-onset diabetes, but also assessed adverse events and return to normal glucose control.
At a median follow-up of 3 years, 524 (25%) of 2093 participants in the placebo group and 475 (22.7%) of 2097 in the vitamin D group had new diabetes. discovered that it had occurred.
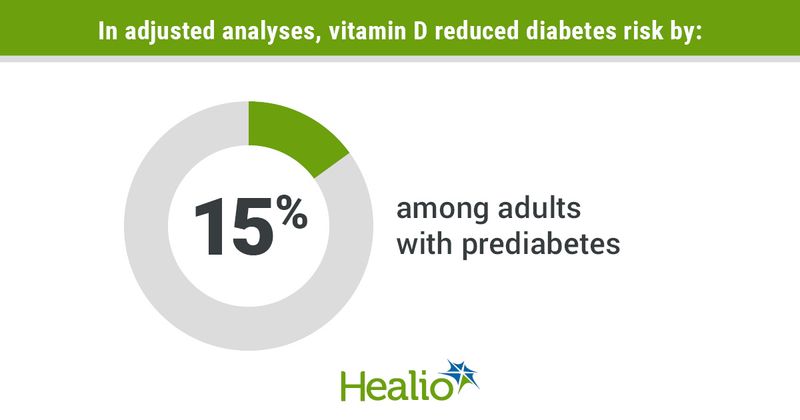
In an adjusted analysis, they wrote, vitamin D reduced diabetes risk by 15% (HR = 0.85; CI 0.75-0.96) and 3-year absolute risk by over 3% (95% CI 0.6-6). ing.
Furthermore, Pittas et al reported that vitamin D increased the likelihood of returning to normal glucose control by 30% (rate ratio = 1.3; 95% CI, 1.16-1.46).
“In addition to slowing the progression to diabetes, a return to normal glucose control is also important because euglycemia is associated with microvascular disease, renal disease, and a lower prevalence of retinopathy,” they wrote.
The researchers also found that cholecalciferol reduced the risk of diabetes by 76% (HR = 0.24; 95% CI, 0.16-0.36) and the 3-year absolute risk by 18.1% (95% CI, 11.7-24.6). I also mentioned that I let Participants in the vitamin D group who maintained mean serum 25-hydroxyvitamin D levels of at least 125 nmol/L during the study maintained between 50 and 74 nmol/L during follow-up.
“Achieving and maintaining higher serum 25-hydroxyvitamin D levels among participants treated with cholecalciferol progressively reduced the risk of diabetes,” they wrote. The results are consistent with reports from aggregate meta-analyses that high doses of cholecalciferol are more effective than low doses in reducing diabetes risk.”
Furthermore, they found evidence that obesity suppresses vitamin D bioactivation by CYP2R1, which leads to decreased production of 25-hydroxyvitamin D, suggesting that weight loss upregulates CYP2R1 expression. are doing.
In trials using active analogues of vitamin D that do not require hydroxylation by CYP2R1 or CYP27B1, baseline BMI did not modify the effect, write the researchers. In two studies that administered cholecalciferol on demand, there was an interaction with BMI.Participants with baseline BMI below median (31.3 kg/m2)2) had a 26% reduction in the risk of diabetes with cholecalciferol compared to placebo. However, it “appeared to have no effect” in participants with a BMI above the median.
“Together, these results suggest that the effect of vitamin D on diabetes risk is mediated through its conversion to 25-hydroxyvitamin D by CYP2R1, which is primarily expressed in the liver. However, it is also expressed in several other tissues, including pancreatic B cells, and is then converted to 1,25-dihydroxyvitamin D by CYP27B1 in kidney and pancreatic B cells and other tissues,” they wrote. “This suggests that while cholecalciferol appears to be beneficial in lean prediabetic individuals with intact CYP2R1 bioactivity, there is an excess of vitamin D that is unable to fully convert vitamin D to 25-hydroxyvitamin D.” It is less effective in overweight or obese individuals, which may explain why it reduces the exposure of pancreatic B cells to the beneficial effects of a fully activated vitamin D molecule.”
Regarding safety, there were no significant differences between vitamin D and placebo groups in mortality, hypercalcemia, hypercalciuria, and kidney stones.
“Long-term observational studies that reported on blood 25-hydroxyvitamin D levels and diabetes risk did not report adverse consequences of high levels of 25-hydroxyvitamin,” the researchers wrote. The benefits and safety of D are population-specific, and the balance between benefits and safety needs to be continually assessed as the evidence evolves.”
In a related editorial, Malachi J. McKenna, MD, Endocrinologist at St. Michael’s Hospital and St. Vincent’s University Hospital, Ireland, and Mary AT Flynn, PhD, RD, “Professional groups advising physicians on the benefits and harms of vitamin D therapy have a duty of care to understand advice from government agencies,” said Dr. Dr. Brown University School of Medicine, a clinical associate professor of medicine and a research dietician at Miriam Hospital. There is.”
“They should promote public health recommendations regarding vitamin D intake requirements, 25-(OH)D thresholds, and safety limits,” they wrote. “There is an important difference between supplementation and therapy. Vitamin D supplementation of 10 mcg to 20 mcg (400 IU to 800 IU) can be safely applied at the population level to prevent skeletal and possibly non-skeletal disease.” “Very high-dose vitamin D therapy may prevent type 2 diabetes in some patients, but it can also be harmful.”